
Case Study: Me+U Care Drives Measurable Outcomes in Medicaid Preventive Care Through Strategic Member Engagement
2026-01-12
Results that Me+U Care can replicate for new health plan partners with implementations completed in under 30 days, without requiring IT resources.
Me+U Care, the leading member communication and caregiver engagement platform for health plans, today announced strong results from a recent Medicaid preventive care outreach initiative that delivered measurable improvements in member engagement, care‑gap closure, and SDOH‑supported appointment scheduling.
Setting the Stage
A leading Medicaid health plan partnered with Me+U Care in 2025 to strengthen preventive care outreach and close critical care gaps across its population. Through targeted, compliance‑driven campaigns, the plan achieved meaningful improvements in screenings, vaccinations, and well‑child visits – demonstrating the power of coordinated, human‑centered communication at scale.
The Result: Personalized Engagement at Scale
Even a seemingly modest outreach population can determine whether a health plan meets or misses a critical quality threshold. For many STAR, HEDIS, and state‑specific Medicaid measures, a shift of just a few hundred completed screenings or well‑child visits can move a plan into the next performance tier. That movement directly influences incentive payments, quality bonus revenue, and competitive positioning. By reaching the right members with precision and supporting them through SDOH‑aware follow‑up, Me+U Care helps plans capture the exact lift needed to cross those thresholds.
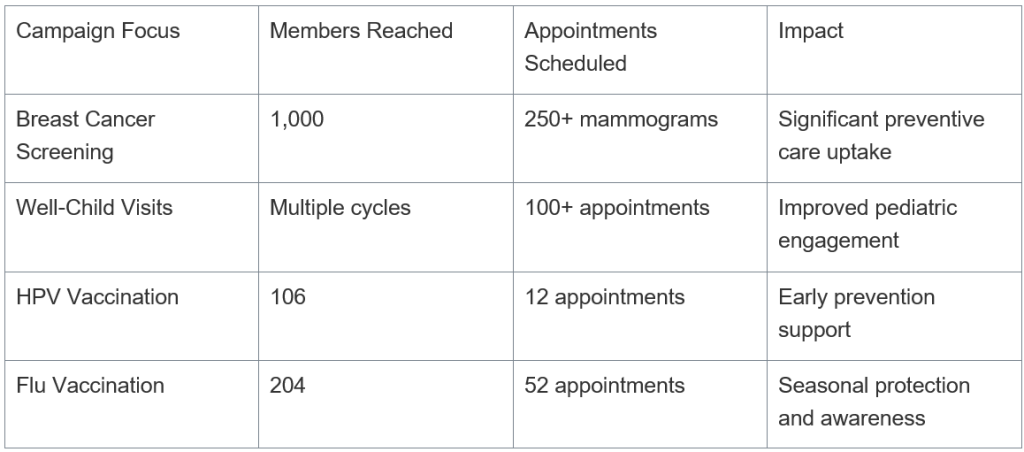
This initiative reached 2,680 members, resulting in 500 scheduled care‑gap appointments supported by social determinants of health (SDOH) assistance. With a 21% overall success rate, the campaign showcased how strategic outreach can drive measurable health outcomes.
A Plan Leader Shared:
“Partnering with Me+U Care allowed us to reach members in ways that truly resonated. The campaigns not only closed care gaps but also reduced barriers by integrating SDOH support. We saw measurable improvements in preventive screenings and well-child visits, underscoring the value of coordinated outreach. These efforts are making a real difference in members’ lives.”
Me+U Care Leadership Perspective
“Health organizations don’t just need more outreach. They need outreach that moves their quality measures,” said Kendall Lockhart, CEO and Founder of Me+U Care. “Our approach is built on the belief that every member interaction should drive an outcome, reduce friction, and strengthen trust. When we help a plan close even a few hundred care gaps, we’re not just improving metrics. We’re improving lives. That’s the impact we’re committed to delivering every day for our clients.”
About Me+U Care
Me+U Care is a plan‑integrated communication and caregiver‑engagement platform that helps health organizations drive outcomes, lower costs, and improve lives. Through compliance‑ready messaging, real‑time engagement, and caregiver‑supported workflows that can be implemented in under 30 days, with no IT needed, Me+U Care empowers health plans to reach members with clarity, compassion, and measurable impact.
Media Contact
For media inquiries, please contact: press@meucare.com